Is it HA or PCOS?
Hypothalamic Amenorrhea (HA) and Polycystic Ovary Syndrome (PCOS) are two conditions that can cause menstrual irregularities in people of reproductive age. Despite their distinct underlying mechanisms, these conditions often present with overlapping symptoms, which can lead to frequent misdiagnoses, and in some cases, harmful treatment recommendations.
Accurate diagnoses are crucial for appropriate treatment and management. Having an awareness of these conditions is extremely important given that approximately 1.62 million women in the U.S. have HA, and an additional 5-10 million have PCOS.
What is Hypothalamic Amenorrhea?
HA is a condition where menstruation stops because of a disruption in signaling from the hypothalamus, a part of the brain that regulates many basic bodily functions, such as temperature, hunger and certain aspects of reproduction. The hypothalamus releases gonadotropin-releasing hormone (GnRH), which is necessary to initiate the menstruation cycle. When it stops releasing GnRH, hormone production is disrupted, leading to irregular or absent periods.
Reasons why your hypothalamus may stop secreting GnRH include:
Undereating
Poor nutrition
Low body fat
Excessive exercise
Emotional or psychological stress
Oftentimes, it’s a combination of these factors that lead to HA. Your body responds by going into “energy-conservation mode,” prioritizing essential functions (like breathing, keeping your heart beating, brain functioning) and pausing less urgent ones like menstruation.
What is PCOS?
PCOS is a hormone condition that affects how the ovaries function. While the exact cause is unknown, it is influenced by both genetic predispositions and environmental factors like lifestyle, diet and toxin exposure. These factors can interact with genetic vulnerabilities to trigger or exacerbate PCOS symptoms. Although there is no cure, symptoms can be managed through dietary and lifestyle changes or use of medication.
To be diagnosed with PCOS, you must meet at least two of the following three criteria:
Irregular periods - Fewer than nine periods per year, cycles lasting longer than 35 days, or very prolonged periods
High levels of androgens - Androgens are a group of steroid hormones (such as testosterone) that play a role in the development and maintenance of male characteristics. This can lead to excess facial and body hair, as well as acne and male-pattern baldness.
Polycystic ovaries - Ovaries that appear enlarged with multiple small follicles seen on an ultrasound
⚠️ Note: Having polycystic ovaries alone is not enough for a PCOS diagnosis. At least one of the other two symptoms must also be present, which is why misdiagnosis is so common.
Similarities & Differences
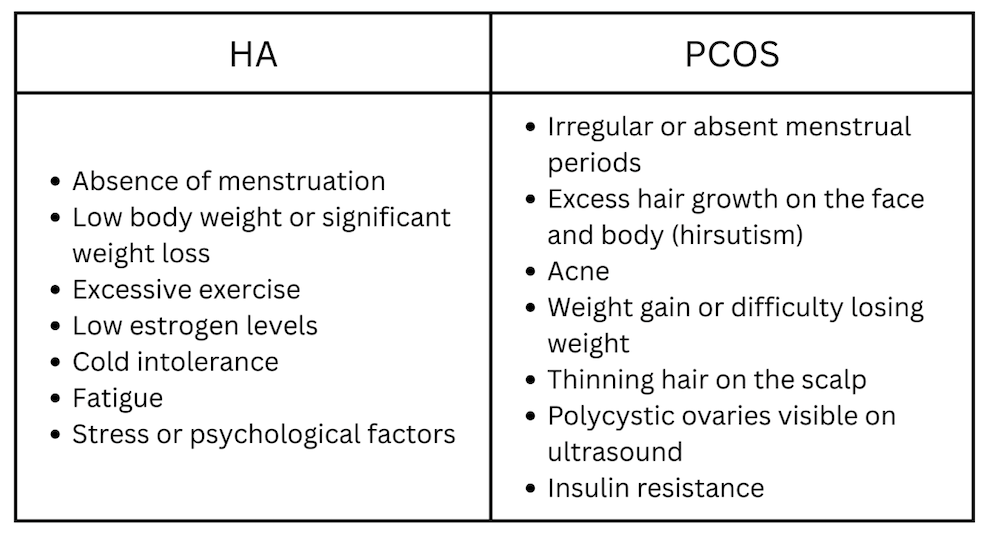
Signs & Symptoms
Diagnosis & Misdiagnosis
To diagnose HA, providers begin by ruling out other common causes of missing periods such as pregnancy, thyroid conditions, or adrenal disorders. Diagnosis typically includes medical history review, physical exam, and blood tests to evaluate hormone levels that influence menstruation. A pregnancy test and a complete blood analysis may also be performed. If you've recently experienced significant weight loss, increased exercise, restrictive eating, or chronic stress, these lifestyle factors are strong indicators of HA.
There is not a definitive test for PCOS. Diagnosis usually involves a combination of symptom tracking, physical examination (checking for signs of androgen excess), and possibly blood tests or ultrasounds. An ultrasound may reveal enlarged ovaries or multiple small follicles, and bloodwork may show elevated androgens or insulin resistance.
Misdiagnosis between HA and PCOS is surprisingly common because both HA and PCOS can present with irregular or absent menstrual cycles and even polycystic-looking ovaries. A key difference lies in the root cause: HA is a functional shutdown due to energy deficiency, while PCOS is a metabolic and hormonal disorder. Getting the diagnosis wrong can lead to ineffective or even harmful treatments.
For example, someone with HA may be misdiagnosed with PCOS if a provider focuses only on the appearance of the ovaries or lack of periods without exploring lifestyle and eating patterns. This is particularly dangerous because the treatment strategies are nearly opposite—HA requires more nourishment, rest, and hormonal restoration, while PCOS often involves insulin management and possibly weight reduction. Misdiagnosing HA as PCOS can lead to further calorie restriction or increased exercise, exacerbating the very issues that caused the problem in the first place.
Long Term Implications
HA poses serious health risks, particularly when it persists beyond six months. In the short term, it signals that the body is under significant physiological stress, often as a result of inadequate caloric intake or excessive exercise.
Long-term estrogen deficiency caused by HA increases the risk of osteopenia, osteoporosis, and stress fractures. It can also impair infertility and may negatively affect cardiovascular health by affecting cardiovascular health due to unfavorable changes in cholesterol and blood pressure regulation. While fertility can be reversed with recovery, some effects, like reduced bone density, may be irreparable if it is left unaddressed for too long.
Check out this Hypothalamic Amenorrhea recovery story: How Tori Got Her Period Back
If left unaddressed, PCOS can lead to a range of long-term health complications. One of the most significant is infertility and a risk to reproductive health. Irregular or absent ovulation makes it difficult for many people with PCOS to conceive without medical support. In fact, some don’t realize they have PCOS until they begin trying to get pregnant. Additionally, without regular ovulation, estrogen remains unopposed, which can lead to endometrial hyperplasia and even endometrial cancer over time.
PCOS is also closely tied to insulin resistance, which can progress to type 2 diabetes if unmanaged. This is why early lifestyle and dietary interventions are so important. Heart health can be affected as well. Chronic inflammation, elevated androgens, and metabolic dysfunction increase the risk of high blood pressure, unfavorable cholesterol levels, and cardiovascular disease.
Both HA and PCOS can significantly affect long-term health, fertility, and quality of life, which is why early intervention and tailored treatment plans are critical.
Treatment Options
HA is primarily treated through lifestyle changes: increasing calorie intake, reducing exercise intensity, and managing stress. Many patients are encouraged to work with a multidisciplinary team, such as a doctor, dietitian, and therapist, to restore hormonal balance and support menstruation.
PCOS treatment may involve hormonal contraceptives to regulate menstrual cycles, and reduce androgens, and address symptoms like acne and hirsutism. Insulin-sensitizing medications like metformin can also help by addressing the insulin resistance at the core of many PCOS cases. Lifestyle changes such as eating a whole foods diet, engaging in regular exercise, and stress reduction can help regulate hormone levels and reduce long-term health risks like diabetes and heart disease.
While HA and PCOS can share some similar symptoms, the causes and treatments are vastly different, and mistaking one for the other can do more harm than good. HA is a condition of energy deficiency as a result of one’s lifestyle, while PCOS is rooted in hormonal and metabolic imbalance that’s caused by a mix of genetics and environment. That’s why accurate diagnosis through a comprehensive evaluation of symptoms, lifestyle factors, and medical history is so important, and it's crucial to work with a provider who understands the nuances of both conditions.
Your menstrual cycle is a vital sign for your overall well-being, not just your reproductive health. Listening to what your body is telling you and getting the right diagnosis is the first step toward long-term health and healing.
Ready to gain more 1:1 support to help you in your healing journey? Apply for private coaching to work with Emily, a Registered Dietitian who helps women world-wide with period recovery & creating a healthy relationship with food, body image and exercise!