How Restrictive Dieting Wrecks Your Gut and Hormones
See Part 1: The Hormone-Gut Connection Every Woman Should Know
When you consistently under-eat, your body interprets this as a threat to survival and shifts into “battery-saving” mode. To preserve energy, it downregulates non-essential systems like reproduction. This leads your ovaries to stop producing sufficient levels of estrogen and progesterone, resulting in hypothalamic amenorrhea (HA), the loss of your menstrual cycle due to dysfunction in the hypothalamus (the brain’s hormone command center). HA not only affects fertility but also impacts bone health, cognitive function, and cardiovascular risk.
Leptin, a hormone produced by fat cells, drops when body fat or food intake is too low. Leptin plays a crucial role in signaling the hypothalamic-pituitary-gonadal axis, which regulates the production of reproductive hormones. When leptin is low, this axis slows down, suppressing ovulation and lowering estrogen and progesterone levels. This can lead to irregular periods, infertility, and other symptoms of low estrogen like low libido or mood swings.
In response to calorie restriction, your body increases the production of cortisol, your body’s main stress hormone. Cortisol naturally goes up and down, but chronically elevated cortisol levels impair gut motility (leading to constipation or diarrhea), alters gut microbiota composition, and increases gut permeability (or “leaky gut”).
This creates a cycle where elevated cortisol → disrupted gut microbiome → more inflammation → more cortisol production. This loop can lead to mood disorders, anxiety, depression, and worsened PMS symptoms.
How Low Food Variety Hurts Your Gut
Restriction isn’t just about how much you eat, it's also about what you eat. The bacteria in your gut need fiber, resistant starches, and polyphenols, which are mainly found in plant foods, to survive and thrive. The fewer foods you eat, the fewer microbial species you support. Chronic dieting often leads to a low-fiber, nutrient-poor diet, which means reduced microbial diversity.
Low microbial diversity is associated with:
Poor estrogen metabolism (via disruption of the estrobolome)
Increased inflammation
Lower immune function
Higher risk for hormone-related conditions like PCOS, endometriosis, thyroid dysfunction, and insulin resistance
A lack of food diversity often leads to key micronutrient deficiencies that directly impact gut function and hormone regulation. Some of the most critical deficiencies that may occur include:
Zinc, Selenium, and Iodine: Crucial for thyroid hormone production
Iron, B12, and Folate: Support menstrual health and energy metabolism
Magnesium and Omega-3s: Help reduce inflammation, regulate cortisol, and support hormone balance
Without these nutrients, your body struggles to maintain hormonal equilibrium, repair the gut lining, and eliminate excess estrogen, increasing your risk for digestive issues, PMS, estrogen dominance, and thyroid dysfunction.
Recognizing and supporting a healthy gut
There has been so much fear-mongering on social media in recent years warning of “leaky gut,” “chronic inflammation,” and “ways to heal your gut,” often linked to a new product or supplement that you need to buy immediately. The truth is, most of these products won’t actually help, and some may even make things worse. The first step is knowing if there’s something even wrong in the first place.
One of the simplest ways to support a healthy gut is to eat enough, and enough variety, especially carbs and fats. As discussed, energy restriction suppresses hormone production, and eating a limited number of foods may mean you’re missing out on essential nutrients.
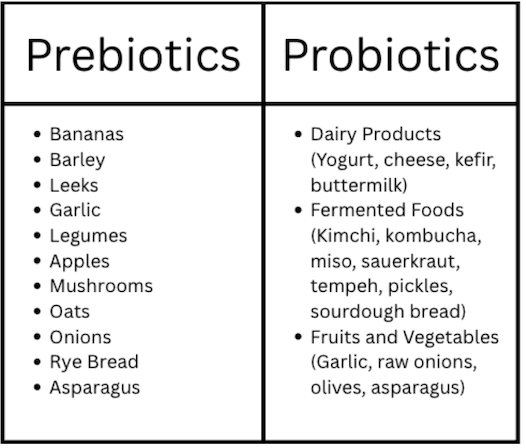
Additionally, prebiotics and probiotics are two key parts of food that support gut health:
Probiotics are live bacteria found in certain foods that provide numerous health benefits. They support the balance of bacteria in your gut and can help increase beneficial microbes while decreasing harmful ones.
Prebiotics are high-fiber foods that serve as the “food” for probiotics, allowing them to grow and function properly.
While both can be taken in supplements found in your neighborhood drug store, the best way to get prebiotics and probiotics are through whole foods:
The Bottom Line: Feed Your Gut, Balance Your Hormones
Your gut and hormones have a very interdependent relationship, and what you eat determines the health of both systems. From regulating your menstrual cycle to shaping your mood, metabolism, and digestion, your hormone health is inseparable from your gut health. Rather than following the latest TikTok trend or fad supplement you keep seeing on Instagram, the most important thing that you can do is return to the basics: eat enough, eat a wide variety, manage stress (to the best of your ability), prioritize sleep, and respect your body’s cues. Supporting gut health through nourishment, not restriction, is one of the best investments that we can make in our long-term well-being.
Looking for 1:1 support?
We help clients inside Nourished to Thrive with personalized nutrition support to help you navigate the best fueling strategies for you and your lifestyle. From healing hormone struggles, digestive issues, and improving your relationship with food & exercise - you will be working with a Registered Dietitian to help you make sustainable changes to support your body long-term!